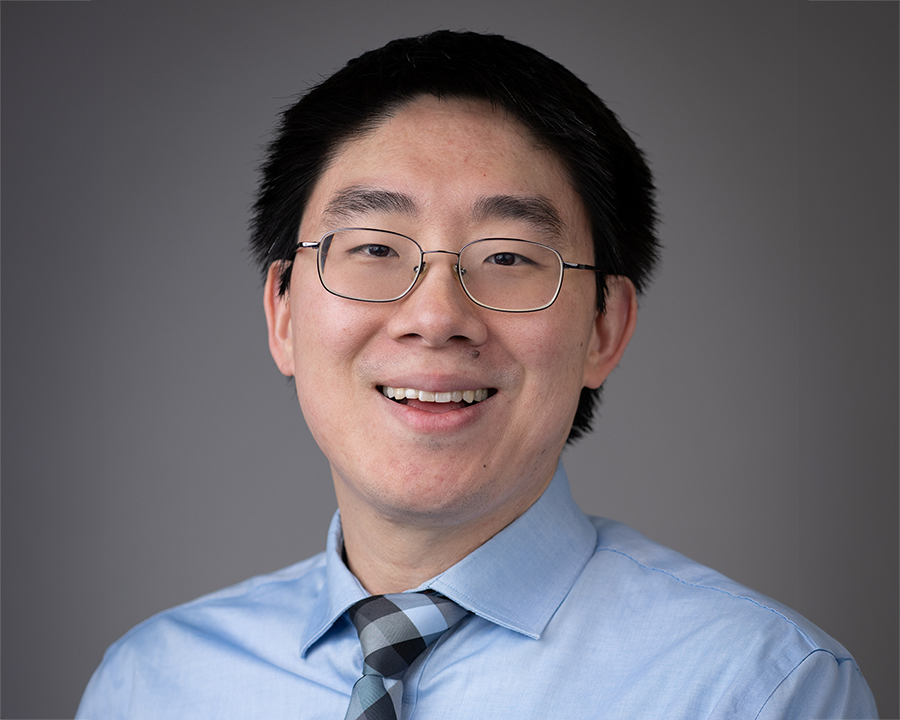
I wear several different hats. I serve as director of the Children’s Medical Center Research Institute at UT Southwestern, which currently has three labs, including mine. The mission of the institute is to better understand the biological basis of disease so that we can uncover new strategies for therapy. Our focus is at the interface of stem cells, cancer biology and metabolism, where we think there are significant opportunities to achieve groundbreaking advances in science and medicine.
I also have been conducting stem cell research for more than 20 years, and I currently oversee the work of about 20 scientists who are studying the molecular mechanisms that regulate the regeneration of adult tissues and how those mechanisms go wrong in the context of diseases like cancer. The goal of my lab is to improve our understanding of the underlying biology with an eye toward developing new therapies. On a larger scale, I recently was elected to the leadership of the International Society for Stem Cell Research, where I will serve as vice president for 2013-2014, president-elect for 2014-2015, and then president for 2015-2016. ISSCR is the leading international organization of stem cell researchers, with nearly 4,000 members from around the globe. In this context, I get involved in global efforts to communicate and disseminate information about stem cell research, as well as policy issues.
There are three major points I would like to focus on during our discussion that hopefully will allow you to have a better understanding of stem cell research. First, there are many different kinds of stem cells that have different properties, and scientists around the world are working very hard to determine which kinds of stem cells can do which kinds of things to help people. It takes a long time to learn what works, as well as how treatments can be delivered safely and effectively.
Second, there is enormous promise in the field of stem cell research. There are multiple stem cell therapies that I was very skeptical about that have turned out to be very promising, in areas such as spinal cord injury, macular degeneration and heart failure. If you look up the government database of proper clinical trials involving stem cells at clinicaltrials.gov, you’ll find 1,900 trials that are currently open.
The third thing to know about stem cell research, however, is that there are a lot of con artists trying to prey on the hopes of desperate patients by setting up clinics in countries with unregulated medical systems. There’s a phenomenon known as stem cell tourism, whereby patients with debilitating diseases will travel to these countries seeking stem cell therapies that turn out to be nothing more than snake oil. There are many ways in which stem cell research is moving forward, but it takes a lot of time and effort because the solutions all start at the molecular level. If a therapy is only available in countries with weak medical regulatory systems, and not in the United States, Canada or the United Kingdom, that means there is not enough data to establish the safety or effectiveness of the therapy and it is unlikely to be beneficial.
I know you probably have some questions, so I’ll try to do my best to answer them.
How is stem cell research addressing cancer?
In my lab, cancer is one of the areas that we are looking at extensively. One of the distinguishing characteristics of stem cells compared to other cells is that stem cells can replicate themselves and perpetuate themselves throughout life. For instance, we all have stem cells in our skin that make skin cells every day, and when you cut your skin and it heals, that’s because stem cells have been recruited to replace the cells that were damaged. We also have stem cells in our bone marrow that make new blood cells every day, because we have to make new red blood cells to transport oxygen around the body, new platelets that will clot to keep us from bleeding to death if we get cut, and new immune system cells to fight infection. There are stem cells in lots of different tissues.
When I started my lab, it was known that stem cells replicated themselves throughout life, but how it happened at the molecular level was not known. I wanted my lab to study those processes at the molecular level, even though I had a great deal of skepticism about our chances for success. But we have been successful to a degree in understanding some of the molecular mechanisms that allow stem cells to replicate themselves in a perpetual way that other cells can’t. In the process, we found that the same key regulators involved in stem cell self-renewal are also involved in cancer, which highjack the mechanisms that normal stem cells use.
Given that insight, we can learn more about what cancer cells are doing at a molecular level by studying stem cells. Anything we learn that promotes the mechanisms that regenerate stem cells could be used to enhance the repair of tissues after injury. Anything we learn that shuts down those mechanisms might also be able to interfere with what a cancer cell would do, and could represent a new cancer therapy.
The best example of a stem cell therapy that has been used clinically for decades is bone marrow transplantation, in which the active ingredient is blood-forming stem cells. Thousands of lives are saved every year around the world because of bone marrow transplants that take place following treatments for cancer. When we treat cancer with chemotherapy, the first thing that dies are the blood-forming cells, and that has been a limiting factor in how aggressively we can treat cancer. Because of breakthroughs in stem cell research, with a few cancers we can now really ramp up the dose of chemotherapy knowing that the blood-forming system will be destroyed, because we now know how to successfully transplant in blood-forming stem cells to regrow the blood-forming system.
What are some of the more exciting discoveries you’ve made at the Children’s Research Institute?
Much of what we’re currently studying has to do with what’s happening at the molecular level and it’s not very easy to describe in a non-technical way, but we are involved with one type of cancer, melanoma, that many people are familiar with in their own lives or in the lives of their friends or family members.
My lab developed many of the techniques to study the stem cells that give rise to the peripheral nervous system. Those cells are very closely related to the cells that give rise to melanocytes, which confer pigmentation to skin. It is also melanocytes that can be transformed by genetic changes into melanoma.
Melanoma is a particularly bad disease. When someone is diagnosed with melanoma, you have it surgically removed and then return to the doctor every three months or so and hope that the doctor doesn’t find anything. Once it spreads to a certain degree and forms what we call distant metastases, there’s nothing you can do. Melanoma is a particularly bad disease. When someone is diagnosed with melanoma, you have it surgically removed and then return to the doctor every three months or so and hope that the doctor doesn’t find anything. Once it spreads to a certain degree and forms what we call distant metastases, there’s nothing you can do.
We decided in my lab to see if we could take the techniques we had developed studying peripheral nervous system stem cells and apply them to melanoma. We wanted to find out if we could understand which cells are responsible for the growth of melanoma tumors, and why some cells metastasize and others don’t, to see if we could develop new strategies for treating the disease.
Based on some of our earlier work, we were able to take a single melanoma cell from a patient and transplant it under the skin of a specialized kind of mouse capable of growing tumors. From those single cells, the mice would grow a human melanoma, and we could then study the biology of the disease and look for new therapies.
It turned out that the behavior of the melanomas in the mice was predictive of the behavior of the melanomas in the patients. If the melanoma spread efficiently and killed the mouse, it would also eventually kill the patient, and if the melanoma was one that did not spread efficiently in the mouse, the patient was cured by the surgery that had removed the melanoma.
This new knowledge gives us a platform for the first time where we can not only study the underlying molecular mechanisms in human melanomas, but also screen for new therapies. I told my lab team that if we could cure melanoma in a mouse, we would be able to go to the clinical trial stage. One of the first things we did was test a variety of FDA-approved drugs for conditions other than cancer for their capacity to kill the melanoma cells from patients. We found a combination of drugs that not only killed the melanoma cells, but also synergized with one of the therapies currently available for melanoma. We believe we are very close to curing the melanoma in the mice using this technique, which will then allow us to move to clinical trials with patients. But if this specific approach doesn’t work, we already have other strategies in the pipeline right behind it, and we will be relentless in exploiting the biological insights we have to try and deliver new therapies to help melanoma patients.
What are your thoughts about the recently reported stem cell research related to Down Syndrome?
The work taking place related to Down Syndrome is more geared toward understanding the underlying biology. Scientists have taken skin cells from people who have Down Syndrome and have reprogrammed those cells to an embryonic-like stem cell state, which is providing an opportunity to better understand at a molecular level how the extra chromosome associated with Down Syndrome operates. This may lead to opportunities for certain therapeutic interventions to be developed that might be able to reverse some of the symptoms.
There’s much more plasticity among cells than we previously thought. We used to think that development was a one-way street, and during embryonic development everything was unspecialized, becoming more and more specialized as development continued, and that once a cell became specialized there was no going back. With the discovery a couple of years ago by Shinya Yamanaka that adult cells could be genetically reprogrammed to become just like embryonic stem cells, other scientists discovered that one kind of cell could become another kind of cell by turning on the right combination of genes. This has all contributed to totally new strategies of how stem cell scientists are studying and seeking treatments for various conditions, such as Down Syndrome.
What are the potential clinical applications involving adipose stem cells?
A lot of work has been done in recent years taking fat and growing certain kinds of stem cells called adipose stem cells, or mesenchymal stem cells. There are a lot of claims in that area that are hype, quite frankly, but mesenchymal stem cells are good at making certain kinds of cells, particularly related to orthopedic functions. They have a number of properties that are potentially useful, and there are hundreds of clinical trials being conducted using mesenchymal stem cells, but it’s one of the areas where the claims have outstripped the science somewhat.
What are the prospects for stem cells to help cure macular degeneration? This is an area where stem cell research has moved forward in an unexpected way. There are different forms of macular degeneration. One form is called dry macular degeneration, which is caused by the atrophy of a layer of cells behind the retina called the retinal pigment epithelium. When those cells die, the light-sensing cells start dying as well. What we have learned from stem cell research in animal models is that we can replace those retinal pigment epithelial cells by transplantation. There are clinical trials taking place now where they have derived retinal pigment epithelium from embryonic stem cells and transplanted those cells into patients, and there is evidence those patients have improved.
What is the risk that stem cells in their regenerative capacity will grow too much and cause cancer?
Normal stem cells have networks of genes that control their regenerative capacity. Some of the genes promote growth and some oppose growth. There are some diseases in which stem cells proliferate too much, and in those cases we look at the molecular mechanisms to see where we can intervene. There are drugs that have been discovered that can short circuit the ability of certain stem cells to grow too much.
It’s interesting to note that the way in which we balance our pro-growth and anti-growth signals changes as we age. During fetal development, everything is dividing as fast as it can to support the enormous growth that is required to grow a baby. As you become an adult, most stem cells are asleep most of the time, but they reserve the ability to go back into cycle and repair a tissue after injury. As you become even older, your regenerative capacity decreases and it takes longer for the body to heal itself, because your stem cells have turned up the anti-growth signals in an effort to prevent the growth of cancers.
You mentioned at the beginning of your remarks the issue of stem cell tourism and clinics that take advantage of people who are desperate for a cure. What is the scientific community doing to address that issue?
One of the priorities of the International Society for Stem Cell Research is to educate patients about the dangers of stem cell tourism. If your doctor doesn’t have reason to believe that a particular therapy is going to help you, then the chances it will help you are remote. If there are no data from proper clinical trials, then there is no basis to believe a particular treatment will work. Patients would be better off working closely with their doctors to access the best proven therapies that are available. In many cases, the existing therapies are obviously inadequate, which is the reason for the research we do. But with existing therapies that have been tested, we know about their safety and effectiveness, and therefore can make informed and rational decisions about what is most likely to benefit the patient.
Regulatory agencies in various countries are also trying to crack down on specific clinics where there is reason to believe they are selling bogus, or at least inadequately tested, therapies. This includes the United States, China and Italy, to name a few. Some of these clinics are using a treatment based on a kernel of an idea that is untested and unlikely to work. In others, a treatment is nothing more than snake oil — an implausible “therapy” promoted by a con artist who knows that what is being given to the patient is highly unlikely to help them. There are documented cases of patients who have been harmed by these clinics.
What’s the current state of government funding for stem cell research?
Funding for biomedical research in the United States has declined pretty steadily over the last 10 years, and the National Institutes of Health budget has become tighter and tighter. More and more labs are closing down due to a lack of funding. The infrastructure for biomedical research is crumbling as a result of declining federal funding. It’s understandable to some extent, as there are elements of austerity affecting many areas of the budget. The way it is affecting biomedical research is that NIH is funding a smaller and smaller percentage of grant applications that are submitted.
One of the great things about science in America is that it is a meritocracy. There is constant competition to come up with the best ideas and to get the best results. Scientists from all across the country write grant applications based on their best ideas, and the applications all go to the National Institutes of Health to be reviewed by study sections that determine which ideas they think are the best. When I started my career, they typically would fund the top 25% of the grant applications received. Now, they are funding in the single digits. I recently submitted a grant proposal that received a score in the top 8%, but we’re not sure if we’re going to receive funding or not, because some sections are only funding in the top 6%.
One great thing in Texas is that we have the Cancer Prevention and Research Institute of Texas, known as CPRIT, which is investing $3 billion in cancer research over 10 years. It was just reauthorized by the state legislature, and it is a tremendously good thing for biomedical research in the state. CPRIT is not only helping to bolster biomedical research in Texas, it is also changing the landscape across the country. One of the reasons I moved from Michigan to Texas is because of the opportunity to do special things that such dedicated funding allows.
Dallas is also a remarkable community with tremendous philanthropy. One of the reasons that UT Southwestern is one of the greatest medical schools in the world, and Children’s Medical Center is one of the biggest and best children’s hospitals in the country, is the philanthropic support of the community.
Despite lower levels of funding than before, the United States still spends an enormous amount of money on biomedical research, and there are many, many benefits that come from it. It’s important that we continue to use the resources we have to understand and cure disease. Part of that comes from having good science policy in place, but it also requires an informed public, which is why I appreciate the opportunity to participate in events like this one.
It’s hard sometimes to see the progress we are making when you look over a short time frame. When you look over longer time frames of 10 to 20 years, however, the changes in our ability to understand and treat certain diseases are profound. I am convinced that the developments taking place in stem cell research today will change lives for the better in the years to come.