The metabolic differences observed between cancer and normal tissue are often thought to reflect the reprogramming that occurs during cancer formation. 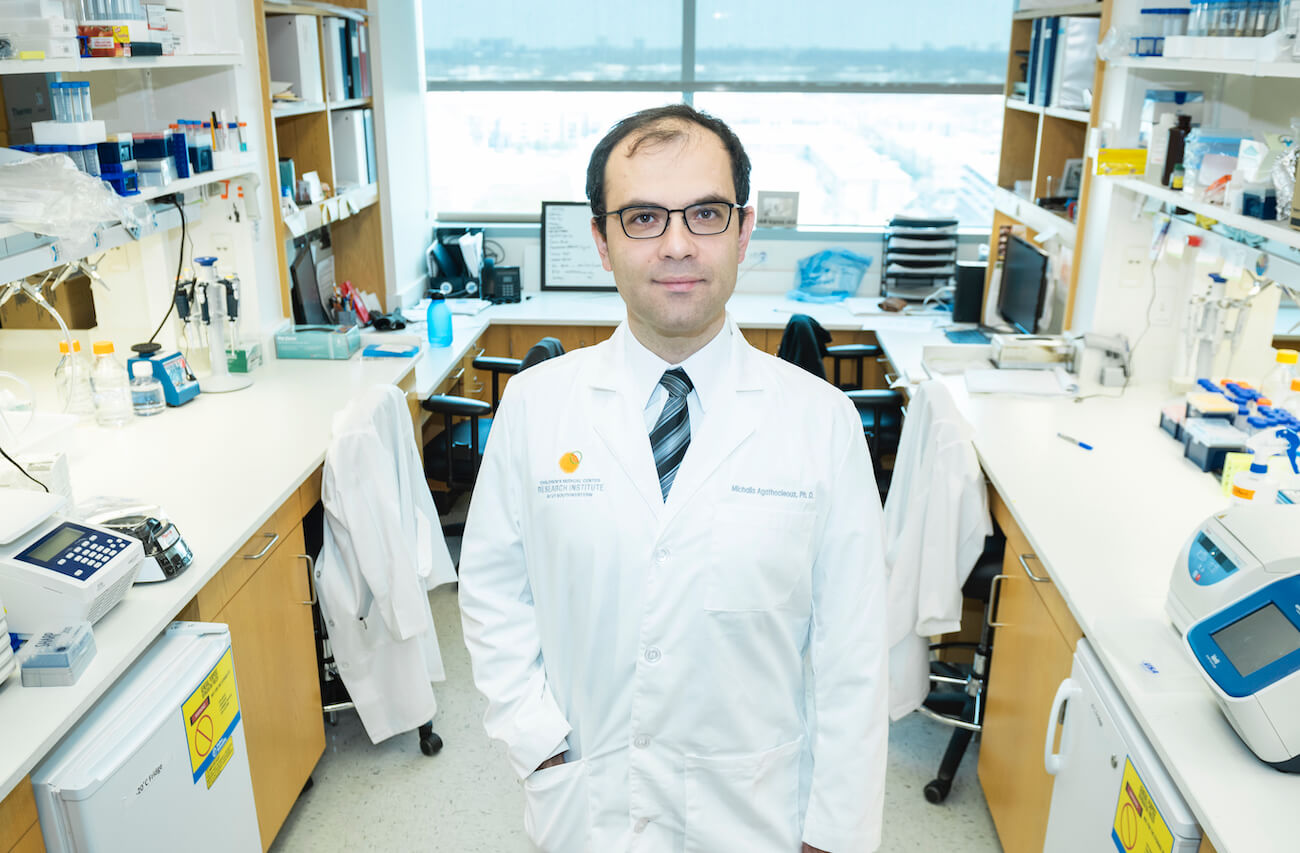 New research from the Agathocleous lab suggests some metabolic features of cancer cells might be inherited from the cell type of origin, usually a stem or progenitor cell. These findings, published in Cell Metabolism, offer a new way to think about cancer cell-specific metabolism and could open new avenues of treatment.
New research from the Agathocleous lab suggests some metabolic features of cancer cells might be inherited from the cell type of origin, usually a stem or progenitor cell. These findings, published in Cell Metabolism, offer a new way to think about cancer cell-specific metabolism and could open new avenues of treatment.
To test the theory that metabolic requirements can be inherited from the normal stem or progenitor cell of origin, researchers used mice to study two types of leukemias that are driven by the same mutation (Pten deletion) but arise from different cells: the first, T-cell acute lymphoblastic leukemia (T-ALL), originates from double positive (DP) T-cell progenitors, and the second, myeloid leukemia or pre-leukemia, arises from blood stem cells (HSCs) or myeloid progenitors. One key difference between the two cell types of origin was how they used glucose. DP progenitors and T-ALL cells used glucose by oxidizing it through the enzyme pyruvate dehydrogenase (PDH), whereas HSCs, myeloid progenitors, and other blood-forming cells did not.
When scientists deleted the PDH enzyme in mice, the number of DP progenitor cells decreased, and the development of Pten-deficient T-ALL was completely blocked. Loss of PDH did not affect HSCs, myeloid progenitors, or the development of Pten-deficient myeloid neoplasms. Together, these findings suggested that the metabolic requirements of these leukemia cells mirror those of the normal stem or progenitor cell of origin independently of mutation that drives leukemia formation. When researchers explored the mechanism by which PDH is required for T-cell progenitor and T-ALL development, they found T-cell progenitors needed PDH to metabolize the high amounts of glucose they were taking up compared with other blood stem or progenitor cells.
“Our results were particularly surprising for the metabolism of HSCs because the current consensus is that HSCs take up more glucose than other blood cells. We set up methods to trace metabolites in HSCs for the first time to understand what nutrients are used by HSCs, and we saw HSCs take up less glucose than other blood-forming cells. Surprisingly, the PDH enzyme is not required for HSC growth or tissue regeneration of most blood cells we studied except for DP T-cell progenitors and the corresponding T-ALLs they produce,” said Michalis Agathocleous, Ph.D., an assistant professor at CRI and lead author on the study.
Currently, comparing cancer cells and their corresponding normal tissue is the standard in the field. However, findings in this paper indicate that if cancer cells and their cell of origin share many metabolic requirements, then these studies could primarily be showing metabolic changes caused by cell-of-origin effects rather than induced by cancer formation. Researchers in the Agathocleous lab suggest it may be necessary to compare the metabolism of cancer cells to the metabolism of their cell of origin, when known, to uncover cancer-specific metabolic features.
Agathocleous is a Cancer Prevention and Research Institute of Texas (CPRIT) Scholar in Cancer Research and an American Society of Hematology (ASH) Faculty Scholar.
This work was supported by the CPRIT (RR180007), an ‘A’ Award from Alex’s Lemonade Stand Foundation for Childhood Cancer, ASH, and donors to the Children’s Medical Center Foundation.