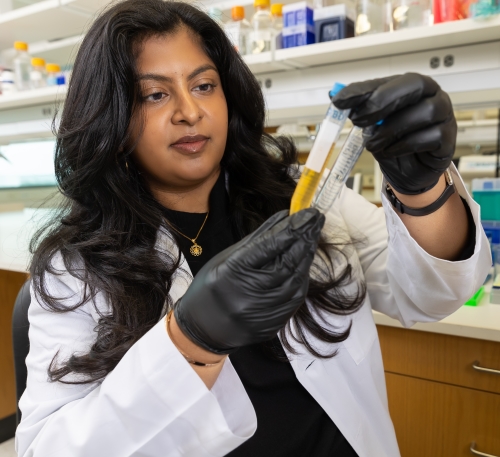
“Divya Bezwada’s discoveries in human kidney cancer have changed the way we think about how these tumors grow and metastasize, and they give rise to a whole series of questions we will try to answer in the coming years,” said the recent graduate’s mentor, Ralph DeBerardinis, M.D., Ph.D., Professor in the Children’s Medical Center Research Institute at UT Southwestern.

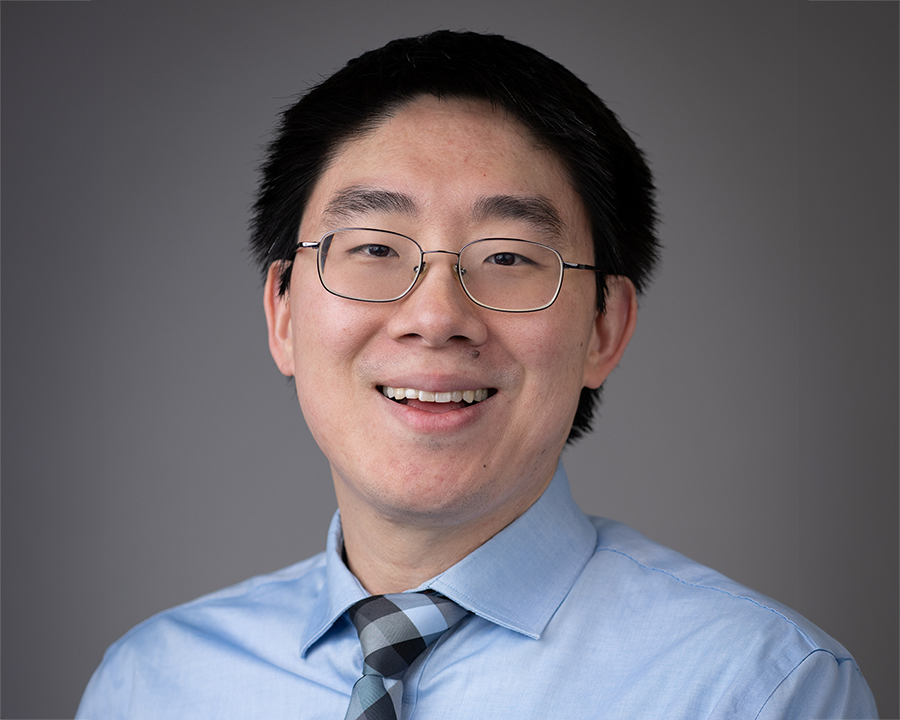
For this work, Divya Bezwada, Ph.D., is the 2023 winner of the Nominata Award, the highest honor bestowed on a student by the UT Southwestern Graduate School of Biomedical Sciences.
It’s remarkable success on an unexpected path. As a college student interested in attending medical school, Dr. Bezwada initially regarded a laboratory as a place to do predesigned work with unsurprising results. Then, in the final semester of her senior year, a professor steered her toward a research lab.
“He saw that I liked discovery,” she said. “It was my first time in a lab where it wasn’t just to check off a required box – it was to really learn something new.”
That spirit has carried her through graduate school and research at UT Southwestern, where she has identified metabolic changes in tumor cells from kidney cancer patients.
“Divya’s project required an exceptional level of creativity, determination, and collaboration,” said Dr. DeBerardinis, also Chief of the Division of Pediatric Genetics and Metabolism, Professor of Pediatrics at UT Southwestern, and a member of the Harold C. Simmons Comprehensive Cancer Center.
This is her second major recognition from the Graduate School; in 2020, she received the Ida M. Green Award for her outstanding commitment to the well-being of fellow students, exceptional community service, and research excellence.
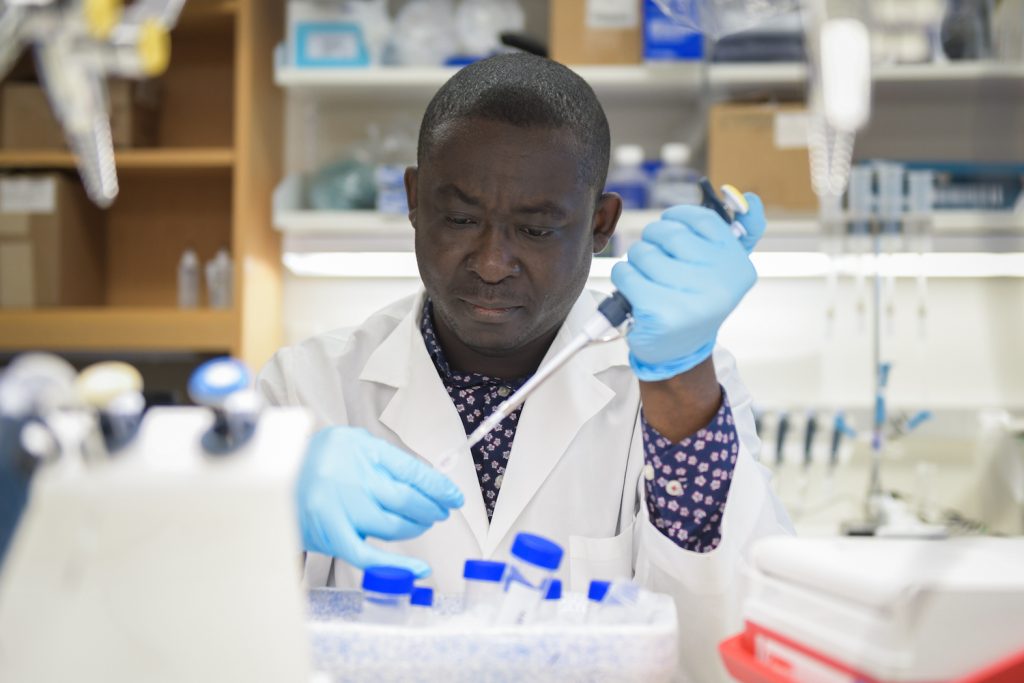
Dr. Bezwada, who graduated in May with a Ph.D. in cancer biology, investigated how kidney tumors use different nutrients to support their growth and survival. The key to tracking the cells’ function was carbon-13 (13C), a form of carbon that’s heavier than the most common type, carbon-12 (12C).
By making nutrients that contain 13C instead of 12C, she could infer how the cell is working by measuring which products of metabolism contain 13C. (For instance, 13C-labeled citrate indicated normal mitochondrial metabolism, while 13C-labeled lactic acid produced in the presence of oxygen showed that glucose is being consumed less efficiently in the cell’s body.)
Dr. Bezwada’s research focused on clear cell renal cell carcinoma (ccRCC), the most common type of kidney cancer. ccRCC cells are known to have a disordered metabolism in culture, but her work is the first to identify how ccRCC tumors use different fuels to support growth in humans.
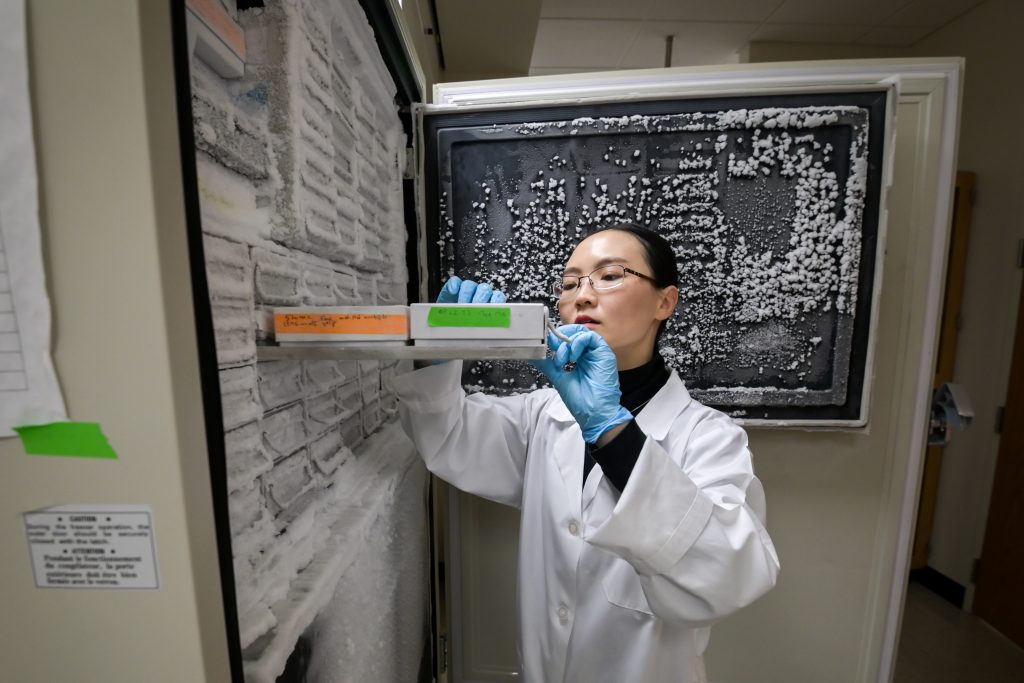
In close collaboration with her clinical mentor, Professor of Urology Vitaly Margulis, M.D., and Urology surgical teams, Dr. Bezwada administered these labeled nutrients to patients who were having surgery to remove kidney tumors. Once the tumors were removed, she froze tissue for analysis and analyzed fresh tissue for oxygen usage, 13C enrichments, and other factors.
The surgery time is long enough for the tumor to pick up the 13C-labeled molecules and metabolize them into 13C-labeled products of metabolism, which Dr. Bezwada could detect through a technique called mass spectrometry. The findings showed that ccRCC tumors suppress a step in mitochondrial glucose oxidation called the TCA cycle. This difference in energy generation in tumors was first described by German scientist Otto Warburg in the 1920s.
Dr. Bezwada’s work marks “the first definitive demonstration of the Warburg effect … in human tumors,” said Andrew Zinn, M.D., Ph.D., Dean of the Graduate School.
She also developed techniques to culture fresh patient tissues and demonstrated that tumor tissues retain their metabolic characteristics outside of the body, indicating that ccRCC tumor metabolism was intrinsic to the tumor.
However, Dr. Bezwada found something surprising when studying ccRCC tumors that had spread to other organs. The metastatic tumors used more glucose in the TCA cycle than primary ccRCCs. This difference in metabolism might be exploitable in preventing or treating cancer spread.
“That’s really the ultimate goal – finding effective therapies for metastatic kidney cancer patients – but we’re well out from that,” she said. “We’re still in the early days of figuring out what causes this difference during metastasis and what’s the critical driver. But our work is an important first step.”
After graduation, Dr. Bezwada will continue her work in cancer and chemical biology as a postdoctoral fellow in the lab of Benjamin Cravatt, Ph.D., at Scripps Research in La Jolla, California.